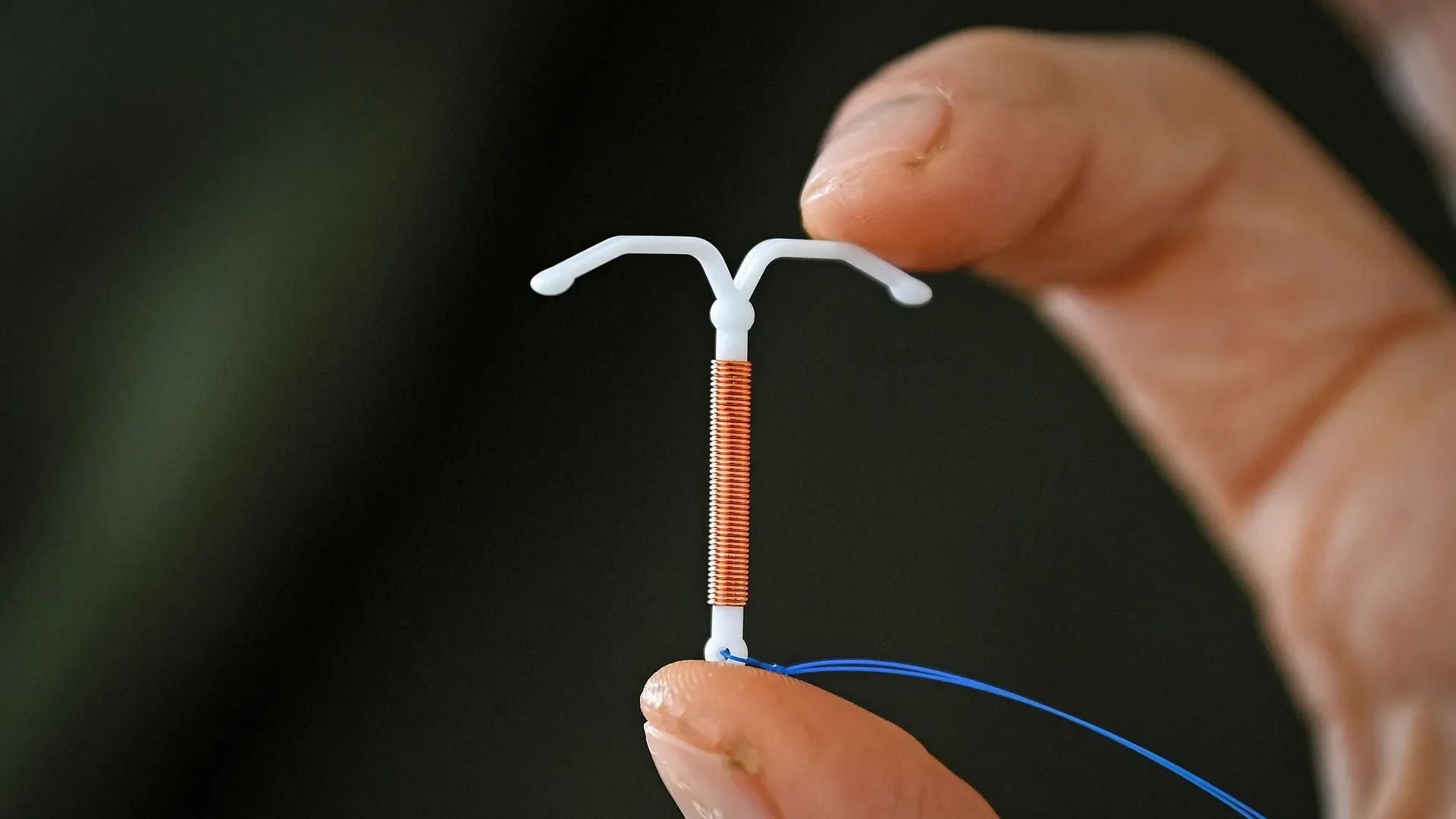
IUD Pain: What to Expect and How to Manage It
By Jade Sisler
Thinking about getting an IUD but nervous about the pain? You’re definitely not alone. Social media has helped normalize conversations about IUD insertions (yay for that)! But it’s also sparked a lot of worry.
Let’s walk through what’s happening during an IUD insertion, why discomfort can happen, and what can be done to make it a smoother experience. Being informed can make a big difference! The main thing to remember is that everyone is different!
Why IUD Insertions Can Be Painful
It’s common to feel pain, cramping, or pressure during an IUD insertion. These sensations usually occur when the IUD passes through the cervix and reaches the uterus. The insertion of an IUD involves several steps that can trigger pain responses. Research shows some specific moments tend to be more painful for individuals. These include placing the tenaculum (a tool that holds the cervix to stabilize the uterus), uterine sounding (measuring depth) and then deploying the IUD.
A big part of it is that your uterus simply isn’t used to having something new inside, so it might respond with cramping as it adjusts.
Pain perception during IUD insertion may also be influenced by:
Age and whether you’ve given birth before
Anxiety or muscle tension
Anatomical difference (e.g., a tilted uterus)
Prior trauma
How much pain someone expects to feel
What Can Help Before, During, and After
At Bridgercare, we know IUD insertions can be both physically and emotionally challenging, so we offer several options to help make the experience as comfortable as possible.
Before the procedure:
Taking a non-steroidal anti-inflammatory drug (like ibuprofen or naproxen) ahead of time can help reduce post-procedure cramps.
Talking with your provider about pain expectations and what will happen helps reduce fear and muscle tension.
Anti-anxiety medication: we can provide a pre-procedure medication to help reduce anxiety (if you choose this, you’ll need someone to drive you home afterwards).
During the procedure:
*If Bridgercare is not your provider, they might have different options than this
- Cervical numbing: we offer two types of numbing for the cervix- a paracervical block (which is a lidocaine injection into the cervix) or topical anesthetic (applied directly).
- Emotional and Personal Support: Bring someone with you to your appointment! They can stay in the room during the procedure, if you want them to! You can listen to music, use your phone, or take deep breaths.
After the procedure:
It’s common to have cramping similar to period pain for a range of time depending on person. For some people, it may last a few hours after they get their IUD, and for others, it may last on and off for a month or so. Your usual methods for relieving period pain can provide relief!
The Bottom Line
Getting an IUD can be all of these things: empowering, painful, exciting, and scary. The insertion process is temporary, and there are lots of ways to make it more manageable.
Talk openly with your provider about your concerns, ask them to explain the process, and discuss all of your pain relief options.
With the right preparation and support, you can navigate your IUD insertion with confidence. To learn about alternative birth control options, click here.